Our secure inpatient service model of care and professional practice sets out how teams will continue to deliver a great experience for patients, carers and families and how we will ensure staff feel valued and motivated.
The model has been created with staff and patients. It supports our trustwide goals set out in Our Journey to Change.
Download a one page summary of the model of care and professional practice Download the model of care and professional practiceModel of care and professional practice
Secure inpatient service 2021 to 2023
Foreword
Introduction
Mission statement and pledge
Our Journey to Change
Section 1 – Model of care
Clinical model of care
Compassion focused trauma informed care
Relevant resources – compassion focused trauma informed care
Our community
Staff resilience and wellbeing
Our definition of success
Relevant resources – our community
Safety, containment and stabilisation through DBT Skills
Relevant resources – DBT skills 1
Exploration, regulation and change
Relevant resources – exploration and change
Relational model
Relevant resources – relational model
Baseline training and supervision for substantive staff
Relevant resources – supervision and training
Section 2 – Patient needs in SIS
Patient needs in SIS
Relevant resources – patient needs in SIS
Section 3 – Professional excellence
Professional excellence
Section 4 – Collective leadership
Our community – collective leadership
Section 5 – Investing in our people
Investing in our people
Ward accreditation
Foreword
The secure inpatient service (SIS) is on an improvement journey. It is aligned with Our Journey to Change while still recognising the unique needs of our staff, patients and their families and carers.
This model of care sets out how teams will continue to deliver a great experience for patients, carers and families and the actions staff need to take to make sure that’s everyone’s experience of the service.
It has been created by engaging staff and patients and has enabled SIS to develop a clear vision for how we deliver care to our service users and how we will care for our staff.
Introduction
We are committed to improving the outcomes and experience for all our patients, their carers and families.
This model presents and describes the key components of our clinical and professional practice approach to the delivery of high-quality care. It does not replace existing models used to understand patients’ presentations, support formulations or direct care plans. This model does not replace existing therapy models or provision of specialist care. Rather, it forms the basis of consistent care that can be expected by patients across the medium and low secure services. It strengthens professional practice and outlines how we support, motivate and develop staff to deliver the best possible care through:
- relational working
- continued professional development
- supervision
- reflective practice
The support given to staff will enhance confidence and competence of working within the complexity of forensic services, inspiring best practice and provi
ding a great place to work.
The Trust values of respect, compassion and responsibilities are our golden threads by which we deliver our care and care for each other.
Mission statement and pledge
Mission Statement: To help people to lead safer, healthier, meaningful and hopeful lives.
Our pledge to patients: To support and care for you with respect and compassion by listening to you and involving you in the planning of your care. We will help you to lead a healthy life whilst in hospital and upon discharge into the community.
Our Journey to Change
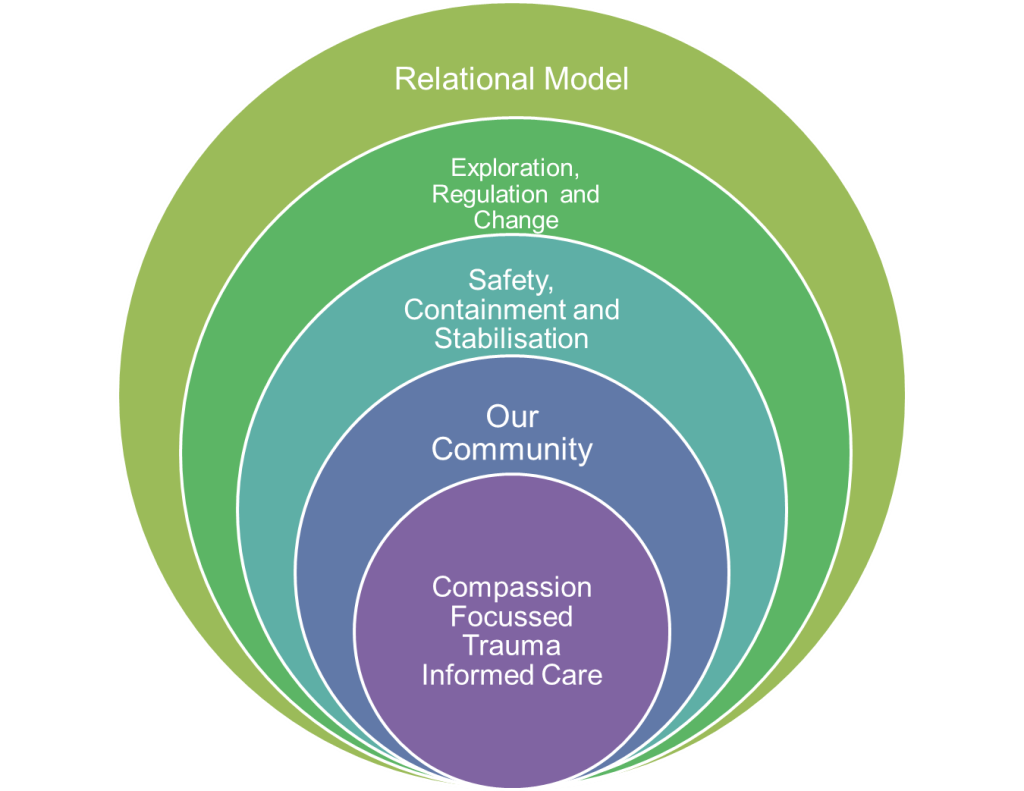
The SIS model of care and professional practice consists of a core component outlining what we pledge to deliver. Visually this is represented as interrelated circles representing our therapeutic pathways that culminate in the delivery of compassion-based care. This core component is our model of care. It is supported by a model of professional practice under 3 key headings:
- Professional excellence
- Collective leadership
- Investing in our people.
Our professional practice model describes how we will deliver the model of care by setting specific objectives within the excellence in care section. Collective leadership will be at the heart of everything we do, and we aim to develop a program of shared governance professional councils to enable the voice of the staff to shine through and be heard by senior colleagues. Finally, a detailed plan for how we will recruit, support, involve and develop and retain our staff is presented under the heading of investing in our people.
The SIS model of care and professional practice is created alongside Our Journey to Change. It describes our intention to support people to lead their best possible lives, the important way we will support patients, their carers and families, and our staff by living our values and our commitment to the thee big goals over the coming years.
Section 1 – Model of care
Clinical model of care
The following shows a diagrammatic proposal of our Clinical Model of Care. It aligns the culture and organisational development work that has been undertaken in 2021, the CAT Relational framework which commenced in 2010 and fundamental and consistent training expectations for staff.
Compassion focused trauma informed care
At the very heart of our service is a compassion focussed approach. The wellbeing of service users and staff is fundamentally what drives us to have this as a ‘golden thread’ across all teams. Understanding how compassion relates to reducing distress is essential for working in a trauma-informed way. Regulating emotions and subsequent behaviours (the premise of DBT) works best when individuals can recognise distress and where it comes from. CFT is grounded in the understanding of the basic emotion regulation systems – threat, drive and safety. These models complement each other and form the psychologically informed interconnecting model across SIS.
All services will be responsive to understanding trauma, how symptoms are manifested and through training and reflective supervision, our staff group will have the confidence and competence to work effectively and safely with individuals with trauma histories and presentations. We can offer specific governed therapeutic interventions which are evidenced to address trauma, ie, EMDR, DBT prolonged exposure, but as a baseline all staff will receive appropriate training and supervision to understand and respond appropriately to trauma presentations. We ensure that service delivery and model of care is trauma-informed, including consideration of assessment documents and use of the Trauma CLiP where appropriate. Through collaborative formulations and care planning we actively involve service users in their care and treatment, ensuring attention and consideration is paid to trauma responses and vicarious trauma experienced.
Whilst CFT was developed as an intervention for people with severe and enduring mental health problems, many of whom had high levels of shame and self-criticism, it has been shown to be an effective approach and understanding for formulations and subsequent management of service users, and in particular those who with trauma histories. The CFT model aims to help promote mental and emotional healing by encouraging people to be compassionate toward themselves and other people. Compassion, both toward the self and toward others, is an emotional response shown to be an essential part of wellbeing with evidenced benefits of improved mental and emotional health. CFT is not a standalone therapy, but is used in conjunction with governed therapies such as CBT, DBT, etc.
What to expect:
- All staff, including those in non-clinical roles, will have an awareness of the CFT model and teams will be supported to embed compassionate responses into their work through training, supervision and reflective practice.
- All services will be curious to the impact of childhood and adult adversity on mental health and suffering. They will understand how traumatic experiences can influence all aspects of functioning ie, relational, physical, emotional/psychological, social and occupational.
- All services will be responsive to understanding trauma, how symptoms are manifested and through training and reflective supervision, our staff group will have the confidence and competence to work effectively and safely with individuals with trauma histories and presentations.
- As a baseline all staff will receive appropriate training and supervision to understand and respond appropriately to trauma presentations. We ensure that service delivery and our model of care is trauma-informed, including consideration of assessment documents and use of the Trauma CLiP where appropriate.
- Every ward/team will have TiC ambassadors that will advocate and embed TiC principles and TiC supervision will be offered monthly on a rotational basis for all wards to support and sustain cultural changes around TiC. Staff will understand the need for curious enquiry around adversity and trauma to ensure that trauma is identified at the earliest point in a client’s journey and to ensure that their treatment plans reflect any unmet needs.
We are committed to reducing iatrogenic harm and through supervision and harm minimisation training have regular conversations with staff regarding this. Therefore, all staff will undertake harm minimisation training (Trust and forensic modules) to assist in the reduction of iatrogenic harm and re traumatisation.
Relevant resources – compassion focused trauma informed care
You will find all relevant resources on the trustwide shared drive > SIS model of care
This includes:
- Trauma CLiP
- Trauma booklet
- Compassion focused care
Our community
The culture and environment in which we live and work forms the basis of all we do. It is crucial that this provides a supportive environment where people can learn, grow, respond and adapt to their surroundings in a healthy and functional way.
The key characteristics of the wards foster:
- a sense of belonging and acceptance – the nature and quality of the relationships is central, and diversity is embraced and not a barrier to progression
- recognition that people have different skills/strengths and we offer an opportunity for people to try new things
- facilitation and encouragement for hope for the future
- opportunities for development for all – training, learning new skills, influencing change
- communication – we recognise that people will communicate in different ways
- there is structure to the day – opportunities to engage in purposeful and meaningful activity
- clear leadership – there is collective leadership and the primary task and purpose of the community is understood by all
- boundaries – expectations of behaviour are clear, understood and regularly reviewed
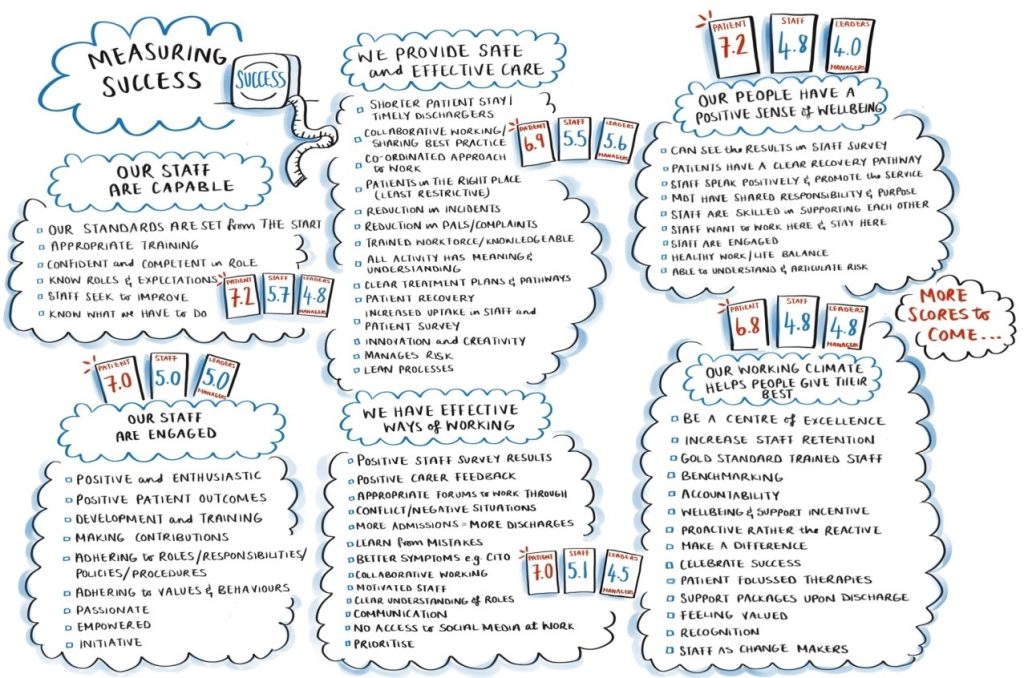
As a staff team we are committed to providing and enhancing:
- safe and effective care
- effective ways of working
- a working climate where people can give their best
- people are engaged
- people are capable
- positive sense of wellbeing
The following is what staff and service users said was important to them. We can keep measuring this.
We regularly assess the social climate on each ward specifically to address how well we provide the following:
- Patient cohesion – the extent to which support amongst peers is typically seen, with scores giving an indication of whether or not characteristics of a therapeutic community exist or not. Items measuring this dimension include the patients care for each other, and there is good peer support among patients.
- Experienced safety – identifies how people view their environment in terms of violence and aggression, and ultimately how they view their personal safety and the safety of others. This is measured using statements such as, there are some really aggressive patients on this unit, and, really threatening situations can occur here.
- Therapeutic hold – aims to recognise if patients feel that they have support on the ward from staff. This is measured using statements such as, staff know patients and their personal histories very well, and, staff members take a lot of time to deal with patients.
The Essen Climate Evaluation Schema (EssenCES – Schalast, 2007) is used to measure social climate. This was originally designed to measure the social climate in psychiatric and correctional settings and then developed to assess essential traits of the social and therapeutic atmosphere of forensic psychiatric wards. It assesses the premise that there is a significant relationship between the social atmosphere on a ward and treatment outcomes (so, the more contained, safe and therapeutic, the better the experience and outcome for service users).
The EssenCES is administered to both staff and service users and it is useful to see if there are any discrepancies between how each other may view the three areas above. If staff report that the ward is safe but the service users don’t, then it gives managers an opportunity to unpick that – is it about complacency, lack of engagement with service users, bullying etc.
The EssenCES lends itself to being repeated (suggested six monthly, although more frequent evaluation may be considered for areas in difficulty) and the data collected allows for the examination of trends, to identify if/where extra resources may be needed and to examine individual patient differences which can be considered and addressed in MDT meetings.
The EssenCES will be administered over a rolling 12-month programme as follows:
| Month | Administration to take place | Report to be available |
| January | Lark Kingfisher Jay | Kestral/Kite Newtondale Ivy/Clover |
| February | Sandpiper harrier/Hawk | Lark Kingfisher Jay |
| March | Linnet Mandarin Northdale | Sandpiper Harrier/Hawk |
| April | Brambling Merlin Thistle | Linnet Mandarin Northdale |
| May | Nightingale Swift Mallard | Brambling Merlin Thistle |
| June | Kestral/Kite Newtondale Ivy/Clover | Nightingale Swift Mallard |
| July | Lark Kingfisher Jay | Kestral/Kite Newtondale Ivy/Clover |
| August | Sandpiper Harrier/Hawk | Lark Kingfisher Jay |
| September | Linnet Mandarin Northdale | Sandpiper Harrier/Hawk |
| October | Brambling Merlin Thistle | Linnet Mandarin Northdale |
| November | Nightingale Swift Mallard | Brambling Merlin Thistle |
| December | Kestral/Kite Newtondale Ivy/Clover | Nightingale Swift Mallard |
Reports and reporting mechanisms
The reports will provide data on:
- Patient cohesion (as rated by patients)
- Experienced safety (as rated by patients)
- Hold and support (as rated by patients)
- Comparable patient scores for the above
- Patient cohesion (as rated by staff)
- Experienced safety (as rated by staff)
- Hold and support (as rated by staff)
- Comparable patient scores for the above as rated by staff
- Compared actual average scores for patient cohesion, experienced safety and hold and support
- Comparable previous data bi-monthly on each of the three domains
The report will also include suggestions for how to improve social climate as identified within each area. Reports will be produced by higher assistant psychologists and supervised by a registered applied psychologist. They will be made available for all relevant staff within ward and service management tiers and discussed in MDT meetings and Ward Improvement Groups (WIG). Ward teams will identify areas of concern and actions needed to mitigate and will be expected to hold these actions locally and detail within a social climate action log.
A full-service report will be produced by the psychology team on a bi-annual basis (January and July) detailing temperature of ward areas, areas of concern and actions taken to address. This report will be submitted to QuAG for service oversight.
Staff resilience and wellbeing
As a service we are committed to supporting the wellbeing and resilience of staff. Resilience relates to people’s ability to stay positive, even when the going gets tough. There are clear links to morale, wellbeing and engagement. To support staff wellbeing we commit to providing six situational requirements in the workplace:
Informed and equipped: individuals feel that they have the information and resources they need to do their work.
Collaborative approach: individuals feel encouraged and supported by their work relationships
Well managed change: individuals experience change as positive and well managed.
Balanced workload: individuals feel their workload is stimulating but manageable.
In control: individuals feel they have control and influence over how their work is done.
Sense of purpose: individuals have a sense of purpose and feel that their goals are clear, challenging and achievable.
We have committed to a psychological contract which outlines how we have agreed to conduct ourselves at work:
We understand what we are trying to achieve together:
We will focus on collaboration, connecting, communication, building trust and valuing diversity of opinion so that people feel heard, involved, they buy in and feel valued.
We will do what we say and manage our time:
We will not lose sight of the need to change ways of working, we will nip problems in the bud before they become big ones and we will take ownership and accountability.
We will role model the change we want to see in the service:
Sifting the narrative away from blame towards appreciation, building consensus, securing buy in and ownership of action. We always seek to understand being comfortable that we might not always agree, but knowing we will always listen and challenge. We will be compassionate: being kind to ourselves as well as others.
We are self aware:
We know as leaders and managers how it feels to be on the receiving end of me. We will learn from our mistakes: by being objective, acting with integrity, humility and acceptance.
We know not everyone can be in the room when we are making decisions:
So we will establish a buddy system to keep people in the loop even when they can’t be there.
What’s okay:
- We work in close collaboration with patients, carers and families – actively engaging with patients at the earliest juncture to ensure an optimum bespoke package of care can be delivered, in as short a period of time as possible, with as little disruption to their life and that of their family as is achievable. We carefully manage the balance between challenge and support in the way we work and the way we care
- We work as a team: supporting and encouraging each other, regularly checking in and doing thorough handovers. We question, challenge and often respectfully disagree with each other, so that we get it right.
- We stick to what we have agreed, and we are always on time. We tell it as it is: if we make a mistake, we own it and say sorry; if we don’t get a job done on our shift, we hand it over; if we don’t know the answer, we find out.
- We say thank you, give feedback and offer praise for a job well done. When something isn’t right, we call it out. We greet each other, welcome people onto the ward, introduce ourselves, show people around and ask how we can help. We smile, say please and thank you. We answer the phone with our name and the name of the ward.
- We focus on solutions and not problems, helping each other to think differently by listening to opinions other than our own. We tackle conflict quickly, explaining why decisions were made so people can accept and work with them.
What’s not okay:
- We don’t focus on the past nor do we ignore, dismiss, manipulate or talk down to each other.
- We don’t come in late and leave early. We never cut corners. We don’t ask staff to work outside of the scope of their practice without training, support or preparation. We don’t walk off site if we don’t get our own way. We don’t ignore patients or staff because we are on our phones, on social media or reading the paper. We don’t leave jobs to other nurses.
- We don’t gossip, criticize others, spread rumours, laugh at people, tut, roll our eyes or walk off when we are being spoken to. We never stand by, let things happen and do nothing. We don’t stab people in the back, swear, shout, mutter under our breath or slam doors. We don’t air our dirty laundry or make negative comments about the service in front of patients. We don’t treat patients like children. We don’t ridicule and humiliate people, interrupt or aggressively gesticulate to emphasize our view. We don’t threaten, manipulate or insult each other. We don’t glare, point fingers, blame, sigh or sulk.
- We don’t raise our voices, argue, shut each other down or dismiss each other’s views. We don’t make decisions without consulting people who will be affected by those decisions.
In essence, we do not make judgements or assumptions about why our patients react to certain difficult situations in ways we may not understand, we do not stigmatise or use de-humanising language, and we speak to each other and patients with kindness, compassion and respect.
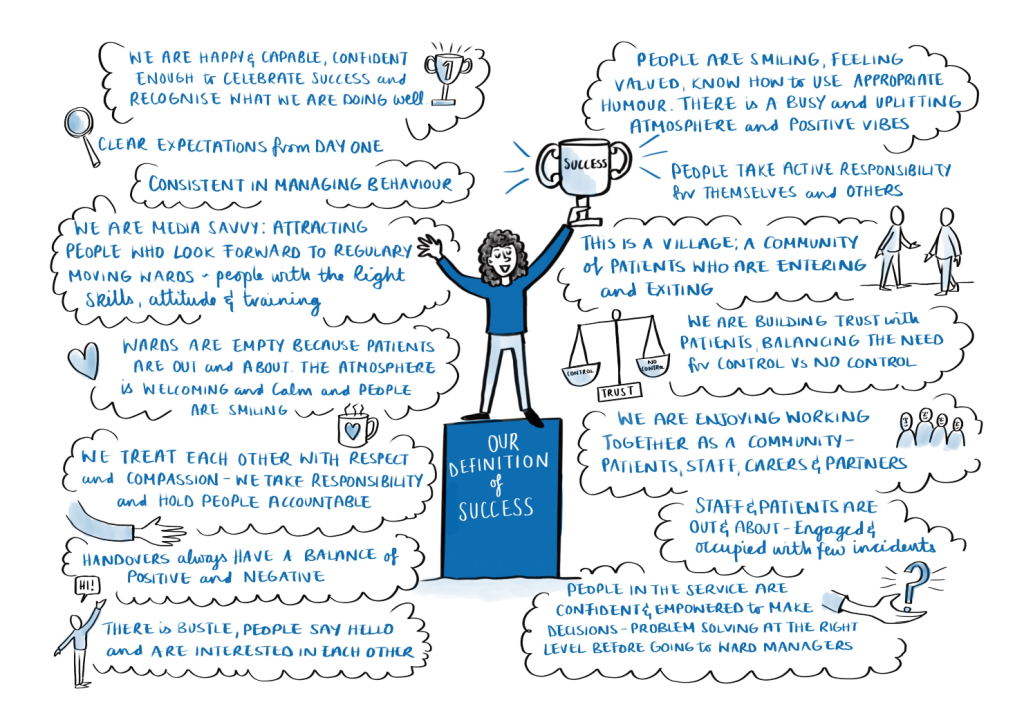
As a collective, we have agreed the facets and behaviours by which we are able to measure our level of success. Essentially, this is defined by collective leadership, providing a great experience for our patients, a great place to work for staff, and an environment by which we display and receive the values of respect, compassion and responsibility.
Our definition of success
Relevant resources – our community
You will find all relevant resources on the trustwide shared drive > SIS model of care
This includes:
- Staff wellbeing guide
- Social climate scale
- Secure inpatient service induction
- Secure inpatient service welcome pack
- Closed culture
Safety, containment and stabilisation through DBT skills
Dialectical Behaviour Therapy (DBT) is a therapeutic treatment technique designed for the treatment of those individuals with borderline personality disorder however is also shown to be beneficial for those with over-controlled behaviour and other relational difficulties. The overarching DBT goal is to help to create for the client a life worth living.
DBT is based on a bio-social theory of borderline personality disorder which sees it as a consequence of an emotionally vulnerable individual growing up within a particular set of environmental circumstances which is referred to as an ‘invalidating environment’.
There are four primary modes of treatment in DBT, of which 1, 2 and 4 are offered within forensic services:
- Individual therapy
- Group skills training
- Telephone contact
- Therapist consultation
The overarching treatment model in SIS is DBT. We will provide a common pathway for intervention across all services, ensuring continuity and consolidation of skills for service users. Using an evidence based and governed therapy framework to address emotional and life-threatening behaviours, therapy interfering behaviours and quality of life interfering behaviours we can deliver group and individual interventions. Short-term behavioural targets can include decreasing suicidal and self-harming behaviours. This uniformed approach helps those moving between wards to have a sense of commonality and understanding and it helps the transition into the community teams. In addition, this consistency provides safety and empowerment which directly links to the trauma informed care approach.
Relevant resources – DBT skills
You will find all relevant resources on the trustwide shared drive > SIS model of care
This includes:
- DBT awareness
Exploration, regulation and change
In line with the NHS Long Term Plan, service users will have improved access to evidence-based therapies and these will be delivered by individuals with appropriate competences and supervision. We will provide evidence-based care and availability of consistent, boundaried and non-judgemental support.
We have a clear understanding of medical and psychosocial therapies recommended by NICE, have identified pathways of stepped-care and also have an evidence base for addressing offending and risk behaviour, again with clear pathways articulated and ensuring effectiveness and efficiency and alignment to length of stay.
Relational experience, in particular the availability of consistent, boundaried and non-judgemental support, is essential and maintained through staff training, supervision and reflective practice.
We offer a range of governed psychological therapies, including CBT, CAT, DBT, EMDR, Schema therapy and Art Psychotherapy. Many GPTs are enhanced through CFT-based interventions. We also offer structured individual and group therapy to address offending behaviour.
We use a range of occupational therapy models and interventions to support improvements in occupational performance centred around the areas of self-care, productivity and leisure.
In SIS, speech and language therapists support people to understand all their communication and eating and drinking strengths and needs.
We also have registered dietitians who assess, diagnose and treat dietary and nutritional problems, guide and support people to make appropriate lifestyle and food choices. They are supported by nutritionists who are qualified to provide information about food and healthy eating.
All therapeutic interventions and treatment pathways are supported by the social work team who use co-production and a strengths-based approach to promote the rights, strengths and wellbeing of service users and carers throughout the treatment pathway – from admission and through to discharge into the community.
Our desired outcomes overall are to:
- reduce risk behaviours
- improve wellbeing and encourage a healthy lifestyle
- improve prosocial living
- reduce the likelihood of re-offending
SIS adopts a recovery orientated approach and by working collaboratively with service users and carers we strive to make continued improvements throughout the service.
The central facets of the recovery approach are to give hope and develop goals for the future, and help individuals to plan for a life worth living through:
- Building a meaningful and satisfying life, as defined by the person themselves
- Recognising that recovery does not occur in isolation but through social inclusion
- Discovery of a personal identity that is separate from illness or disability
- The recovery and outcomes team support recovery through:
- Service user and carer involvement opportunities
- Opportunities for co-production
- Events and opportunities for engagement that link to the CHIME factors
- Forums to provide feedback for continued service improvement
- Service user and carer engagement in research and development
- Training for those in expert by experience positions to support and influence meaningful change
Relevant resources – exploration and change
You will find all relevant resources on the trustwide shared drive > SIS model of care
This includes:
- Governed Psychological Therapies Guide
- SLT
- Dietetics
- Occupational Therapy
- Recovery and outcomes
Relational model
The literature and key national documents highlight the importance of staff training and a model for reflective practice – the benefits of this for frontline staff are widely recognised. In addition, national reports (including the Mid-Staffordshire and Winterbourne enquiries) highlight the importance of a culture and way of working that promotes compassionate care across the system and the leadership challenge of enabling a culture which allows people to speak out and challenge practice. Therefore, a reflective culture does not start and finish with frontline staff. This requires an awareness of the relational dynamics at all levels of the organisation.
An overarching relational model based on cognitive analytic therapy was introduced into the forensic service in 2010 and has been supported through training and ongoing regular reflective practice for frontline staff working on the wards. More recently this model has been enhanced and supported through additional theoretical models of art psychotherapy, group analysis and schema therapy. Outcomes for frontline staff include: increases in staff perception of their understanding of patients, and their confidence in relation to patients as well as reduction of perceived stress.
Within relational models, it is helpful to understand the context of dynamics within and for organisations. Both servicer users and staff are operating within the wider context of the organisation and the role of senior leadership teams has been identified as crucial in setting the culture of the organization. The relational dynamics between leaders, managers and their teams can impact on team functioning, individual wellbeing and patient care. A relational model as applied to organisations can hold different perspectives and dynamics in mind by acknowledging the part that I bring to the interaction, the dynamics between myself and others and the dynamics in the wider organisation, culture and political and social climate.
Aims of the relational model
The purpose of training in the forensic service is:
- To give a common relational language for understanding interactions on a day to day basis in order to aid reflective practice
- To develop skills in mapping interactions and the relationship between staff and patients
- To enable reflection on dynamics we might get pulled into
- To reflect on how ways of interacting might elicit certain responses
- To consider different ways of responding to achieve a different outcome
- A relational understanding of trauma and complexity
- Increasing awareness of our own personal relational dynamics
- Increasing awareness of relational dynamics in the team/organisation
All staff will be given an opportunity to engage in relational awareness training and undertake reflective practice. In summary, the training introduces the concept that every interaction is influenced by the three-part rule; one part brought by the individual themselves, one part by the patient or other staff member in the interaction and one part by the system within which they are working. Reflective practice encourages staff to consider these dynamics in understanding the challenges within the workplace, whether in relation to patients, managing staff or managing relationships within the wider system/organisation. This allows staff to identify any unhelpful dynamics and to consider if they want to make changes to the way a situation is managed.
Relevant resources – relational model
You will find all relevant resources on the trustwide shared drive > SIS model of care
This includes:
- CAT overarching relational model
- CAT awareness
Baseline training and supervision for substantive staff
Workforce development is one of the three key priorities underpinning and supporting the clinical model of care. Training, reflective practice and supervision is designed to help staff to think about, and where necessary, alter their attitudes towards people within secure services and to develop the skills and confidence of staff in working with people with complexity.
All staff will have an opportunity and be expected to undertake awareness training within the first six months of employment in the following:
- Trauma-informed care
- Compassion focused care
In addition, all frontline staff will be expected to undertake the following training within their first 12 months of employment:
- Mindfulness
- Two day introductory relational training (CAT)
- DBT skills
- Resilience and wellbeing training
The resilience and wellbeing training was developed in 2014 and continues to be facilitated on a regular basis across the health and justice region. It is a practical and thought provoking look at what resilience is and how to develop it in oneself and others.
The training introduces wellbeing as made up of two key concepts: feeling good and functioning well. It highlights that resilience is the ability to cope with life’s challenges and adapt when faced with adversity.
To support staff personal and collective resilience, training will be offered to all staff to support wellbeing. Resilience helps people to maintain their wellbeing in difficult circumstances. Research has shown that high levels of wellbeing and resilience don’t just lead to fewer mental health problems (such as stress, depression) but also are associated with:
- Improved learning and academic achievement
- Reduced absence from work due to sickness
- Reductions in risk-taking behaviours like smoking
- Improved physical health
- Reduced mortality
- Increased community/organisational involvement
To improve staff wellbeing and resilience the training programme considers and introduces techniques that can be introduced into personal and work lives. The aims and objectives of the course are:
- To describe the concept of resilience and how this relates to well-being at work
- To think about critical occupations and who is most at risk
- To give an overview of the three motivational systems within compassion focussed therapy consider and how this relates to wellbeing
- Reflect on the time we have received compassion and how this improved wellbeing
- To develop a personal action plan
All staff will be offered an opportunity to attend resilience training within the first 12 months of employment. ESR role specific training has been approved for those working within SIS. There is a need to ensure all team members employed within SIS be suitably qualified and have a thorough understanding of patient need to ensure we provide the best possible patient care across the service. To support this, a review of training currently available with the Trust has been undertaken and several courses identified to support awareness, competency and professional development. These courses are additional role specific training for all staff working within the service.
| E-learning | What to search for on ESR |
| ADHD theory | 346 online introduction to adults ADHD |
| Autism theory | 346 online autism introduction |
| Dementia | 000 dementia awareness |
| Mental health and ageing | 346 online mental health and ageing E&T only |
| Dual diagnosis | 346 online dual diagnosis theory (15167314) |
| Learning disabilities | 346 online introduction to learning disabilities (15164796) |
| Challenging behaviour LD | 346 online challenging behaviour LD introduction |
| Mental health awareness | 346 online mental health awareness theory |
| Challenging behaviour MH | 346 online challenging behaviour MH introduction |
| Psychosis | 346 online psychosis theory |
| Personality dosorder | 346 online personality disorders theory (15165866) |
In addition to the e-learning training described, face-to-face trauma informed care and resilience and wellbeing training is mandatory and will be reported via ESR.
Clinical supervision underpins the very essence of good care, and it supports clinicians to develop their knowledge, skills and abilities. It is an essential element of clinical governance and embodies professional and personal development, with the overall aim of enhancing clinical and professional practice. Professional regulatory bodies (HCPC, NMC, GMC) support clinical supervision in their respective codes of conduct, in the confidence that clinical supervision is necessary if practitioners are to develop their practice in the best interests of patients. The Care Quality Commission (CQC) outlines clearly what providers should do to comply with the section 20 regulations of the Health and Social Care Act. Outcome 14 is one of the core 16 standards on quality and safety and makes specific reference to supporting frontline staff by ensuring they receive appropriate training, education, professional development, supervision and appraisal; all of which are inextricably linked to clinical governance frameworks.
It is mandatory that all staff be offered and encouraged to participate in the following supervision:
- Work based supervision and management
- Peer supervision
In addition, all frontline staff will be encouraged to participate in:
- DBT consult
- CAT reflective group
Relevant resources – supervision and training
You will find all relevant resources on the trustwide shared drive > SIS model of care
This includes:
- Trauma informed care
- Compassion focused care
- Mindfulness training
- Two day introductory relational training (CAT)
- DBT skills training
- Resilience and Wellbeing training
- Supervision policy
- DBT consult
- CAT Reflective Group
Section 2 – Patient needs in SIS
Patient needs in SIS
The Model of Care assists with effective, evidence-based models of working. It allows for a range of patient needs to be met, including physical health. It is also aligned to NICE guidance, Royal College of Psychiatry recommendations, quality network standards and the Trust’s values and direction. It is recovery focused, patient-centred and supports Our Journey to Change. In addition, the model embraces the principles of trauma informed care, positive behavioural support and allows us to create an appropriate clinical and therapeutic environment to deliver this care in response to clinical need and risk.
The trust’s three big goals, as set out in Our Journey to Change are:
To co-create a great experience for our patients, carers and families so you will experience:
- Outstanding and compassionate care, all of the time
- Access to the care that is right for you
- Support to achieve your goals
- Choice and control
To co-create a great experience for our colleagues, so you will be:
- Proud because your work is meaningful
- Involved in decisions that affect you
- Well led and managed
- That your workplace is fit for purpose
To be a great partner, so we will:
- Have a shared understanding of the needs and the strengths of our community
- Be working innovatively across organisational boundaries to improve services
- Be widely recognised for what we have achieved together
In line with this, there are three specific facets central to our service delivery, aimed to enhance patient, staff and carer experience:
Safety – reducing the risk of harm that someone may pose to themselves or others
Effectiveness – ensuring delivery of treatments is needs led and responsive to these needs
Efficiency – providing treatment in a timely fashion so as not to delay discharge and create long waiting lists and costs
Generally, service users within the secure inpatient service suffer from, although not exclusively, mental illness (including schizophrenia), learning disability, autism spectrum disorders, relational (personality) difficulties and complications arising from substance misuse. Diagnosis is important and it needs to align with the legal detention. However, formulation and understanding of clinical needs from a bio-psycho-social model is important and it is this that will drive clinical care.
We prevent harm by ensuring proportionate and patient centred care planning and that least restrictive practice is observed at all times. The overall aim is to develop an ethos in which people with mental health problems, learning difficulties and autism are able fully to participate in formulating plans for their well-being, risk management and care in a collaborative manner. Consequently, more positive and collaborative service cultures develop reducing the need for restrictive interventions. The impact of these changes would be to improve service user and staff experience and safety indicators on the wards. It is expected that the use of restrictive practices would reduce.
Relevant resources – patient needs in SIS
You will find all relevant resources on the trustwide shared drive > SIS model of care
This includes:
- RCPsych recommendations
- Quality network standards
- Positive behaviour support
- Relational security
- Restrictive practice
- Avoidable harm
- NICE guidance – www.nice.org.uk/guidance
- Our Journey to Change – www.tewv.nhs.uk/about/trust/our-journey-to-change
We also follow a risk-needs-responsivity model and provide the right intervention at the right time by the right person.
The following relevant resources can also be found on the trustwide shared drive:
- Acquired brain injury
- ADHD
- Autism
- Learning disability
- Mental disorder and co-existing substance misuse
- Psychosis
- Relational difficulties
Section 3 – Professional excellence
Professional excellence
To develop the best possible positive practice environment, we are committed to developing and maintaining the clinical and leadership skills of the workforce to ensure:
Exemplary professional practice is evidenced by effective and efficient care services, multidisciplinary collaboration, and high-quality patient outcomes. Staff and patient feedback, analysis of need and alignment with nationally recognised safety priorities enabled the identification of 5 priorities under 4 key headings.
Compassion focused trauma informed care
- Open to the reality of suffering and aspire to its healing.
- Curios and responsive to the impact of childhood and adult adversity on mental health.
Safety, stabilisation and containment
- Provide a common pathway for intervention across all services, ensuring continuity and consolidation of skills for service users.
Exploration, regulation and change
- Evidence based care and availably of consistent, boundaried and non-judgemental support.
Avoidable harm
- Preventing harm by ensuring proportionate and patient-centred care planning.
| Compassion focused trauma informed care | |
| Compassion is defined as capacity to open to the reality of suffering and aspire to its healing. Understanding how compassion relates to reducing stress is essential for working in a trauma-informed way. CFT is grounded in the understanding of the basic emotion regulation systems – threat, drive and safety. Staff need to be curious to the impact of childhood and adversity on mental health and suffering and understand how traumatic experiences can influence all aspects of functioning. Staff need to be responsive to understanding trauma through training and reflective supervision. | What we will do a) Work with service users to design and plan their care and treatment b) Deliver trauma-informed services, including use of appropriate assessment documents and use of Trauma CLiP c) Train staff to provide specific governed therapeutic interventions d) Provide training and reflective supervision for staff to enable them to work effectively, safely and with confidence with those with trauma histories |
| Safety, stabilisation and containment | |
| The overarching treatment model in SIS is DBT. We will provide a common pathway for intervention across all services, ensuring continuity and consolidation of skills for service users. Using an evidence based and governed therapy framework to address emotional and life-threatening behaviours, therapy interfering behaviours and quality of life interfering behaviours we can deliver group and individual interventions. Short-term behavioural targets can include decreasing suicidal and self-harming behaviours. This uniformed approach helps those moving between wards to have a sense of commonality and understanding and it helps the transition into the community teams. In addition, this consistency provides safety and empowerment which directly links to the trauma informed care approach. | What we will do a) Train all front-line staff in DBT skills and give support to deliver skills groups b) Encourage and support staff to attend DBT consult groups to support learning, reflection and professional practice c) Provide DBT resources to each ward/team area |
| Exploration, regulation and change | |
| In line with the NHS Long Term Plan, service users will have improved access to evidence-based therapies and these will be delivered by individuals with appropriate competences and supervision. We will provide evidence-based care and availability of consistent, boundaried and non-judgemental support. | What we will do a) Understanding of and adherence to medical and psychosocial therapies as recommended by NICE b) Have identified pathways of stepped care for a range of MH and LD presentations c) Provide evidence-based interventions to address offending and risk behaviour d) Support a recovery orientated approach to work collaboratively with service users and carers |
| Avoidable harm | |
| Patient safety is the avoidance of unintended or unexpected harm during the provision of health care. We will minimise patient safety incidents and drive improvements in safety and quality to ensure patients are treated in a safe environment and protected from avoidable harm. | What we will do a) Ensure proportionate and patient-centred care planning b) Ensure staff are trained to harm minimisation and iatrogenic harm c) Ensure restrictive practices are used only as a last resort and for the shortest possible time d) Manage serious risks and manage the right balance between care and security through procedural, physical and therapeutic/relational security |
Section 4 – collective leadership
Our community – collective leadership
To provide a living and learning experience for patients and a great place to work for staff we are committed to providing and enhancing a working climate where people can give their best.
Shared governance
- Staff have collective ownership to improve practice; placing staff at the centre of decision making
Empowerment
- Inclusivity and diversity – your voice is heard
- Psychological contract
Professional councils
- Staff led forums, enabling collective leadership

| Collective leadership | |
| Within our community we aim to empower staff at all levels to develop their personal and team leadership qualities, behaviours and skills. We will implement collective leadership in practice to enable healthcare teams to provide safe and compassionate patient care. Where there is a culture of collective leadership, all staff members are likely to intervene to solve problems, to ensure quality of care and to promote responsible, safe innovation. Acknowledging that our clinicians are often better placed to recognise the need for change, suggest improvements in their everyday roles and play a vital part in their implementation and evaluation. The principles of shared decision making within the clinical environment are instrumental in creating a ‘hive’ of innovation. | What we will do a) Implement a minimum of 3 councils in year 1 b) Implement a minimum of 3 councils in year 2 c) Establish reporting mechanism for new councils d) Seek regular feedback from staff and service users via existing forums and meetings to ensure that staff feel fully informed and engaged to enable to do their job effectively and service users have enough information that continues to facilitate their rehabilitation and they can freely contribute to service developments. |
Section 5 – investing in our people
Investing in our people
To achieve the delivery of high quality care it is crucial we ensure our undergraduate workforce receive effective training, that we proactively recruit highly skilled staff and we work to develop staff and retain skilled and experienced staff. In addition the health and wellbeing of a workforce goes hand in hand with success and productivity levels.
The delivery of high quality patient care requires a motivated and skilled workforce and this requires a multi- faceted people plan that ensures investment in staff whether it be access to education and training, talent management, or wellbeing initiatives. Innovation in models of care delivery and challenging traditional role boundaries should be encouraged in order to meet staff and patient needs
Education
- All staff can reach their full potential
Innovation and service improvement
- Designing workforce models around patient need
Research and development
- Supporting staff at all levels to be curious
Wellbeing and resilience
- Looking after you & helping you when you need it
Safe staffing
- Optimising skill mix and establishments to deliver excellent care
| Education | |
| Education helps people think, feel, and behave in a way that contributes to their success, and improves not only their personal satisfaction but also their community. In addition, education develops human personality, thoughts, dealing with others and prepares people for life experiences. Access to education is linked to higher levels of staff engagement and associated higher performance levels and patient outcomes | What we will do a) Ensure educational components of the SiS Model of care is delivered as described b) Ensure career pathways for all professions c) Complete an annual Training Needs Analysis and align personal development plans with service priorities and produce an annual training and education plan d) Provide equal opportunities for all through Equality and Diversity e) Ensure strategic succession planning is in place f) Ensure leadership and QI training is accessible for all g) Develop a talent management approach with HR and process for identifying and nurturing talent across all staff groups h) Optimise all opportunities to align the priorities of HEIs and clinical services to ensure the best student placements and academic input into our day-to-day practice, embedding model of care and professional practice |
| Innovation and service improvement | |
| Innovation can be referring trying something new or changing an existing process or model. Staff usually have the best ideas and should be supported to try new things and we grow from the experience and what we learn. | What we will do a) To lead and support transformative workforce ideas and changes b) Greater utilisation of non-nursing colleagues to deliver innovative models of care aligned with trust and service objectives |
| Research and development | |
| Research is creative and systematic work undertaken to increase the stock of knowledge but can often be associated with a sense of in trepidation. In healthcare focus is often put on large scale studies, generating income and funding, complex data analysis and highly academic publications. The aim of this approach in secure in-patient services is to encourage all staff to be curious and be supported in all types of research form small scale audit and publications right along to PhD and post-doctoral studies | What we will do a) Exposure: make research available to all staff b) Engage: maximise opportunities for active research involvement c) Educate: to work with Higher Education Institutions (HEIs) to capitalise on research related educational opportunities and develop innovative educational provision for research skills d) Embed: strengthen the infrastructure and governance arrangements to support and embed research at all levels into clinical practice and demonstrate improvements in patient experience and outcomes e) Effective leadership: deliver a constant message at all levels that research awareness, engagement and skills matter and will be supported.a0 |
| Wellbeing and resilience | |
| Wellbeing: the state of being comfortable, healthy or happy is directly linked to the ability to be happy at work and deliver excellent care. | What we will do a) Create a work and learning environment where staff will want to stay and be supported to reach their full potential b) Collective commitment to six situational requirements identified by staff: information and equipment, collaborative relationships, well manged change, balanced workload, in control, sense of purpose c) Enable staff to attend training, reflective practice and supervision d) Provide opportunities for all staff to attend the resilience training e) Collective commitment to the psychological contract developed by staff |
| Safe staffing | |
| Safe staffing can lead to a decrease in preventable harm. It has been found that short-staffing increases staff risk of experiencing burnout which can lead to an increased turnover in employment. | What we will do a) Maintain safe staffing and skill mix b) Monitor the impact of staffing numbers and skill mix on service delivery c) Develop and enable a robust recruitment and retention plan d) Ensure efficient use of resources e) Work with HEIs to agree student numbers |
Ward accreditation
The Trust improvement plan includes the development and implementation of a ward accreditation program.
Experience shows accreditation programmes can drive continuous improvement in patient outcomes, and increase patient satisfaction and staff experience at ward and unit level. Using a collective sense of purpose teams can support communication, encourage ownership and achieve a robust programme which measures and influences care delivery. Furthermore, staff engagement is directly linked with organisational performance and decreasing morbidity and mortality.
In SIS we will be demonstrating our successes by striving to be part of the development and piloting of accreditation programs. More information will become available over the course of 2022/2023.